Simulation in healthcare – optimising the utilisation of a therapy centre with AnyLogic
A major challenge facing hospital directors are the continuously changing framework conditions in the healthcare sector. These demand constant adaption of the hospitals’ operating organization, in order to rectify inefficiencies that may occur in medical-administrative terms as well as being caused by the building design of the medical facilities. Simulation software may help reaching this goal; it can realistically reproduce the complexity and dynamism of hospital routine, by removing the limits of a mere static process view.
In a current project, a process simulation was carried out by the hospital consulting firm ANDREE CONSULT in cooperation with simulation service provider SimPlan in a specialist clinic for psychiatry and psychosomatics. The simulation aimed to show the impact of a variety of factors on the therapy schedule of a psychiatric therapy centre. The initial analysis indicated a high amount of unused therapeutic time, possibly due to insufficient scheduling of the therapy sessions.
Due to the fact that the therapy rooms are not a bottleneck resource and walking distances within the buildings are not a relevant variable, SimPlan set up a “virtual pavilion” to simplify the simulation model, instead of modelling a realistic building plan, as is usually done.
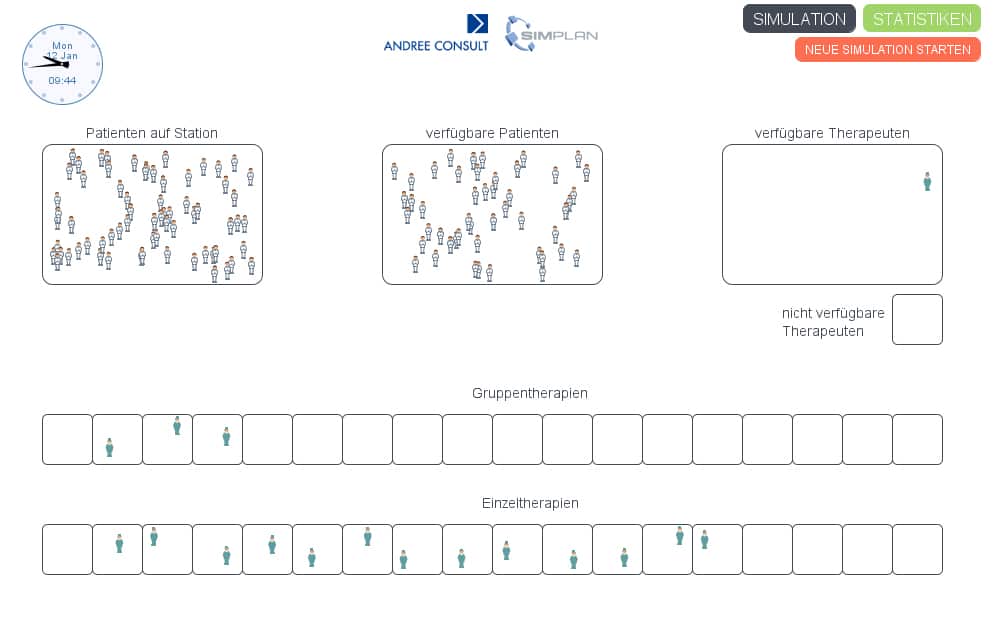
Fig 1: virtual pavilion
The goal was to make the utilization of therapists and patients, required room capacities and billable services transparent, in order to reveal economic resources. The focus of the simulation was on the following questions:
- How high is the therapists’ time utilization and the amount of time not spent on therapies?
- How many therapy rooms are required at most at the same time for individual and group therapies?
- How many individual and group therapies do the patients have in reality, compared to the aimed for target relevant for billing-purposes?
To achieve a service range that corresponds to demand and economic success as well as an optimal utilization of the patients, the number of individual and group therapies per patient per week was defined. Further parameters were the minimum and maximum group size and the limited availability of the patients at specific times. To calculate the time utilization of the therapists and, in turn, the amount of time not spent on therapies, the time needed for preparation and follow-up of the therapies (like documentation and break times) had to be taken into account.
To be able to adapt the simulation to changing framework conditions, the simulation model was given to the client, so they can use it to simulate different scenarios at any given time. The simulation file is usable on any computer, and no purchase of the simulation software is necessary.
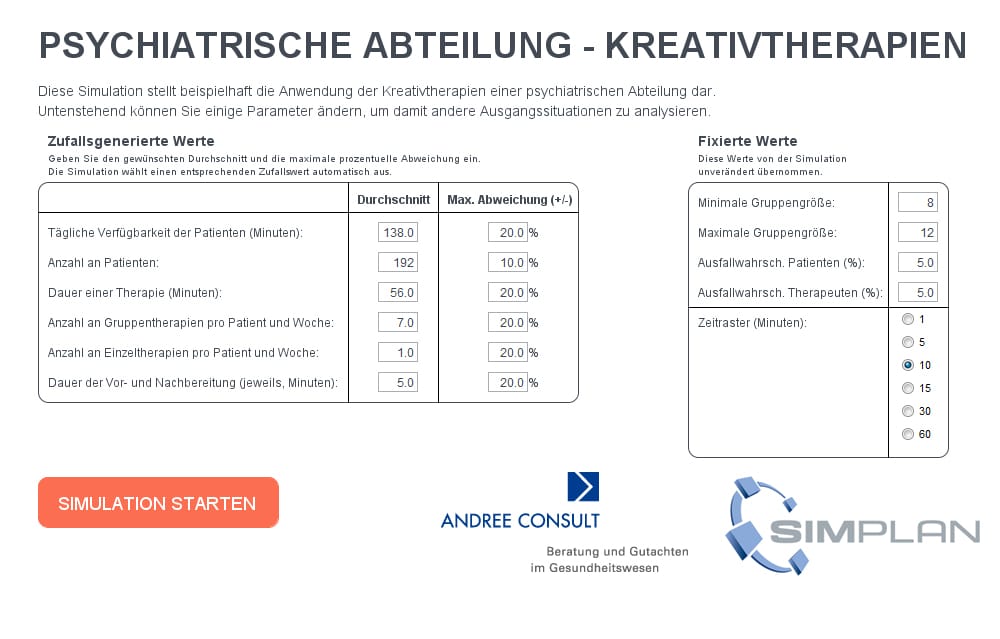
Fig 2: variable parameterisation
As an example, by changing the values of the variable „time grid (minutes)”, the following cause-effect relationships can be simulated in the model:
- The group size of the group therapies
- The maximum room requirements (maximum number of therapies scheduled at the same time)
- The utilization of the therapists
- Therapies not taking place (therapy shortfall compared to the target value)
- The time grid in minutes represents each next possible time window (e.g. 12:00, 12:10, 12:20) when the therapist can start the next therapy session.
Figure 3 gives an overview of the effects of different grid types.
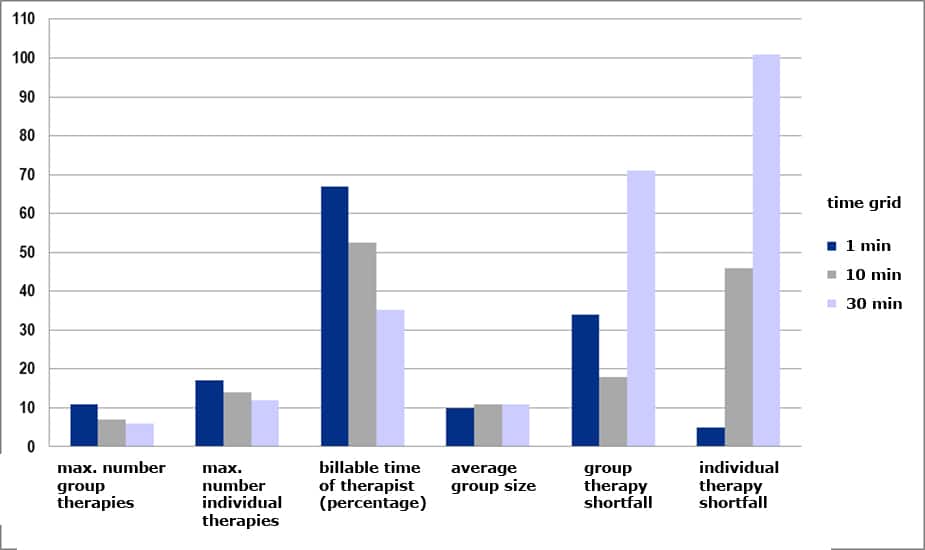
Fig 3: cause-effect relationships of the variable “time grid”
Practical application
The abovementioned example clearly shows the advantages of the use of simulation in health services. It allows for a realistic depiction of the present situation, but also of a possible target situation with improved processes. This leads to insights that cannot or only partly be obtained by other analysis methods, and therefore cannot otherwise be used as a factual basis for decision-making processes.
The great strengths of simulation especially come into play when analysing potential changes of framework conditions, resources or process structures. Parameters can be changed without risk with a few mouse clicks (like the time grid in the example above); room requirements, shift schedules and numbers of patients can be varied, processes can be adapted and much more. A simulation run with changed parameters only takes a few moments and offers the same extensive analysis data as the simulation of the present situation, while never disrupting the running of the actual medical facility at any point in time. This makes simulation an ideal decision support tool in addition to the classic analysis tools and methods.
